PRESIDE
Screening for preeclampsia in the first trimester of pregnancy
Learn more about the PRESIDE research project
Contact us Discover PRESIDE
Learn more about the PRESIDE research project
Contact us Discover PRESIDE
To examine the performance of screening for preeclampsia in the first trimester of pregnancy in an unselected Danish population by combining maternal characteristics, blood pressure, flow in the uterine artery and biochemical markers, and to evaluate the attitude among pregnant women towards this screening.
Contact us BackgroundPreeclampsia is one of the most serious complications of pregnancy, since it is highly associated with morbidity and mortality in both mother and child. The condition, which affects up to 8 % of pregnant women, is defined as hypertension occurring after 20 weeks of pregnancy with concurrent proteinuria (1). Severe preeclampsia is associated with maternal complications such as eclampsia, disseminated intravascular coagulation, acute renal failure, liver failure and pulmonary edema (2). For the fetus/child, the consequences vary from intrauterine growth restriction in moderate cases to intrauterine death in severe cases (2).
The pathogenesis of preeclampsia is not fully elucidated, but abnormal trophoblast invasion is considered to be essential. In preeclampsia, the placental perfusion is reduced, and hypoperfusion and hypoxia leads to oxidative stress in the placenta and to systemic inflammation (7). The condition only occurs in the presence of placenta, and the most effective treatment remains delivery of the baby and placenta. Hence, preeclampsia is the most common reason for induced preterm delivery. Approximately 15 % of women with preeclampsia deliver before 34 weeks of gestation, i.e. very preterm (5), which further increases the risk of serious neonatal complications.
It is well-known that daily treatment with 100-150 mg of acetylsalicylic acid (ASA) during pregnancy may prevent severe preeclampsia leading to delivery before 34 weeks, particularly if treatment is initiated before 16 weeks of gestation (9). Danish guidelines recommend prophylactic treatment with ASA to women who are considered high-risk according to information regarding previous pregnancies and diseases (10). International clinical guidelines recommend treatment with ASA for women who have had severe preeclampsia in a previous pregnancy, have chronic renal disease, autoimmune disease, pregestational diabetes or severe essential hypertension (10). However, this strategy only identifies 36% of cases (11) and the vast majority of women who develop early preeclampsia are thus not offered preventive treatment.
Recent studies suggest that more than 80% of cases of early preeclampsia can be predicted in the first trimester of pregnancy, if maternal history is combined with measurement of blood pressure, flow in the uterine artery and selected biochemical markers such as Pregnancy-Associated Plasma Protein A (PAPP-A) and Placental Growth Factor (PlGF) (15). Results from a recently published randomized clinical trial have shown that treatment with 150 mg of ASA among women, who are screen-positive according to the suggested algorithm for first trimester screening may reduce the risk of early preeclampsia with up to 80 % (27).
Screening for preeclampsia raises both ethical and moral questions (11). What are the consequences of being screen-positive, and which options do women have in relation to a positive screen test? Furthermore, it is important to clarify whether or not it has adverse consequences to be screen-negative such as delayed diagnosis in relation to symptoms of preeclampsia (12). A qualitative study performed in the Netherlands showed that pregnant women in general had a positive attitude towards screening for preeclampsia, and that the feeling of reassurance when the test was negative represented an important incentive for participation in the screening (13).
Before implementation of screening for preeclampsia in Denmark, it is essential 1. To validate performance of the screening model for preeclampsia in a representative low-risk Danish population 2. To evaluate the attitude among pregnant women towards screening for preeclampsia
Contact us MethodsHypothesis:
It is possible to increase the detection rate for early preeclampsia from 36% to 80% through screening in the first trimester of pregnancy.
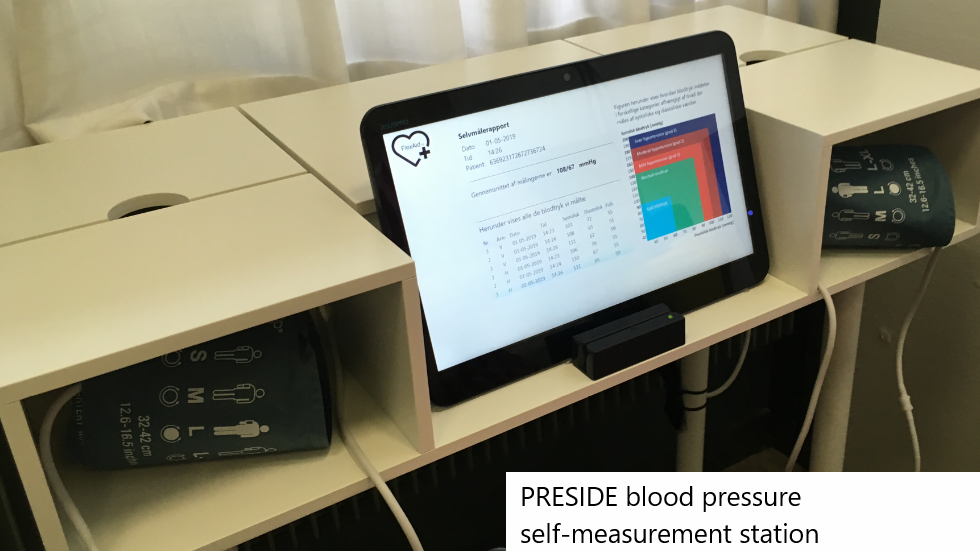
We propose to perform a multicenter study in which five Danish university hospitals will collaborate to recruit pregnant women at the time of their first trimester scan. The women will have a blood pressure measurement as well as measurement of flow in the uterine artery and will be asked to provide blood samples for PlGF analysis as well as an aliquot for analysis of potential new markers. As the purpose of this study is to validate the proposed screening algorithm, we will not calculate the individual woman’s risk of preeclampsia until she has delivered. The pregnant women along with the health personnel will, therefore, be blinded for the risk assessment for preeclampsia. Women, who are considered at increased risk according to the current national guideline based on maternal history, will be offered counseling by an obstetrician and treatment with ASA.
We wish to include 8300 pregnant women in the study. Each year approximately 20000 women deliver at the five participating departments, and each department should be able to include approximately 1700 pregnant women over a recruitment period of 6-12 months. We expect that 3 % of the population will develop preeclampsia (i.e. 250 women). The proportion of women with preeclampsia who deliver before 34 weeks is expected to be 0.3 % (25 women) and 0.7 % (58 women) will deliver before 37 weeks.
Statistical considerations: The current detection rate for early preeclampsia in Denmark is estimated to be 36 % when based on maternal history alone. With the proposed screening program, we expect to detect at least 80 %, i.e. 20 of the expected 25 cases. With an increase in the detection rate from 36 % to 80 %, we would have a power of 90 % (β=0.90) for α=0.05.
Participants:
Inclusion criteria:
Data collection: In relation to the first trimester scan, information regarding age, parity, body mass index, smoking habits, gynecological/obstetrical history, previous preeclampsia and other health issues will be collected via a questionnaire. All information will be entered in Astraia (the national ultrasound database) along with clinical information such as blood pressure and flow in the uterine artery. The collected blood samples will be stored until the women have delivered, where after they will be analyzed for markers of preeclampsia, and the individual risk of preeclampsia will be calculated.
For all participants, information will be collected regarding pregnancy complications, onset of delivery, gestational age at delivery, birth weight and length, neonatal morbidity and mortality as well as neonatal and maternal admittances. This information will be collected from registers and individual patient files.
All information regarding participants will be protected according to the Danish legislation.
Hypothesis:
Pregnant women in Denmark have a positive attitude towards screening for preeclampsia.
Methods: Data will be collected via a questionnaire based on Theory of Planned Behavior (14). The individual questions are phrased (15) with inspiration from the results of a British and a Dutch survey-study (12,13). To ensure that the questionnaire evaluates issues with relevance for Danish women, three interviews with smaller focus groups of pregnant women will be conducted at Rigshospitalet by the applicant. The questionnaire will be validated, and thereby modified, through cognitive interviews with 20 pregnant women at the four other departments that take part in the prospective multicenter study. The final questionnaire will be distributed electronically using SurveyXact. A reminder will be sent to non-responders after one week and women who have not responded after two weeks will be followed up with a phone call.
Design: In order to obtain a representative sample, we wish to include 300 pregnant women. Age, ethnicity, education and pregnancy-related data as well as women who choose not to participate will be registered. Electronically distributed survey-studies typically achieve a response rate around 75%.
Exclusion criteria:
Prediction models may perform differently in different populations (36). It is therefore imperative to examine the performance in a large Danish cohort before the suggested international algorithm becomes nationally implemented in Denmark. This study will examine the performance of the prediction model in a large unselected cohort, which will be representative for a low-risk Danish population and provide the opportunity to determine the appropriate cut-off for high-risk pregnancies in Denmark that would benefit from treatment with ASA. If the study shows that the screening identifies at least 80 % for a false-positive rate of 5-10 % in an observational cohort and women have positive attitudes towards the screening, the next step will be to implement treatment with ASA for women at high risk of preeclampsia according to the model. After a period of 6-12 months it would then be possible to estimate the effect of ASA treatment by comparing this intervention cohort with the observational cohort. If the study shows that the proposed algorithm identifies less than 80% of women with preeclampsia in Denmark, it will be important to adjust the algorithm according to our population. For this purpose it will add significant value to have collected a biobank, which will also provide the possibility to investigate new markers for preeclampsia as well as markers for other adverse pregnancy outcomes such as gestational diabetes. Implementation of screening for preeclampsia will entail extra health care costs in relation to the first trimester screening program due to a need for additional time for scanning as well as analysis of biochemical markers. These extra costs should, however, be set against significant human and economic savings due to fewer maternal and neonatal admittances, if we can appropriately identify women who would benefit from treatment with ASA during pregnancy. The study would therefore also add information for a cost-benefit analysis for screening for preeclampsia since it would be possible to evaluate the necessary resources besides estimating the detection rate and false-positive rate.
Contact us EthicsThe study will be performed in accordance with the applicable regulatory requirements/legislation. Permission to perform the study will be sought from the Danish Scientific Ethical Committee, and the study will be reported to the Danish Data Protection Agency. The women will be asked for permission to draw additional blood samples. The results of the biochemical analyses will not be available for clinicians and participants during pregnancy. Therefore, the participants will not be informed about their individual risk according to the suggested algorithm during their current pregnancy. The women will be asked for permission to store blood samples in a biobank for future studies of biomarkers for preeclampsia and other adverse pregnancy outcomes such as gestational diabetes. This will be optional for the participants and they will be able to withdraw their consent at any time.
Contact us References
1. Roberts CL, Ford JB, Algert CS, Antonsen S, Chalmers J, Cnattingius S, et al. Population-based trends in pregnancy hypertension and pre-eclampsia: an international comparative study. BMJ Open 2011 Jan 1;1(1):e000101.
2. Sibai B, Dekker G, Kupferminc M. Pre-eclampsia. Lancet 2005 Feb 26;365(9461):785-99.
3. Bellamy L, Casas JP, Hingorani AD, Williams DJ. Pre-eclampsia and risk of cardiovascular disease and cancer in later life: systematic review and meta-analysis. BMJ 2007 Nov 10;335(7627):974.
4. Vikse BE, Irgens LM, Leivestad T, Skjaerven R, Iversen BM. Preeclampsia and the risk of end-stage renal disease. N Engl J Med 2008 Aug 21;359(8):800-9.
5. Poon LC, Maiz N, Valencia C, Plasencia W, Nicolaides KH. First-trimester maternal serum pregnancy-associated plasma protein-A and pre-eclampsia. Ultrasound Obstet Gynecol 2009 Jan;33(1):23-33.
6. Ward RM, Beachy JC. Neonatal complications following preterm birth. BJOG 2003 Apr;110 Suppl 20:8-16.
7. Steegers EA, von DP, Duvekot JJ, Pijnenborg R. Pre-eclampsia. Lancet 2010 Aug 21;376(9741):631-44.
8. Redman CW, Sargent IL. Latest advances in understanding preeclampsia. Science 2005 Jun 10;308(5728):1592-4.
9. Bujold E, Roberge S, Lacasse Y, Bureau M, Audibert F, Marcoux S, et al. Prevention of preeclampsia and intrauterine growth restriction with aspirin started in early pregnancy: a meta-analysis. Obstet Gynecol 2010 Aug;116(2 Pt 1):402-14.
10. Hypertension in pregnancy: The management of hypertensive disorder during pregnancy. Nice Clinical guideline August 2010.
11. Akolekar R, Syngelaki A, Sarquis R, Zvanca M, Nicolaides KH. Prediction of early, intermediate and late pre-eclampsia from maternal factors, biophysical and biochemical markers at 11-13 weeks. Prenat Diagn 2011 Jan;31(1):66-74.
12. Poon LC, Syngelaki A, Akolekar R, Lai J, Nicolaides KH. Combined screening for preeclampsia and small for gestational age at 11-13 weeks. Fetal Diagn Ther 2013;33(1):16-27.
13. Velauthar L, Plana MN, Kalidindi M, Zamora J, Thilaganathan B, Illanes SE, et al. First-trimester uterine artery Doppler and adverse pregnancy outcome: a meta-analysis involving 55,974 women. Ultrasound Obstet Gynecol 2014 May;43(5):500-7.
14. Poon LC, Nicolaides KH. Early prediction of preeclampsia. Obstet Gynecol Int 2014;2014:297397.
15. Akolekar R, Syngelaki A, Poon L, Wright D, Nicolaides KH. Competing risks model in early screening for preeclampsia by biophysical and biochemical markers. Fetal Diagn Ther 2013;33(1):8-15.
16. Spencer K, Souter V, Tul N, Snijders R, Nicolaides KH. A screening program for trisomy 21 at 10-14 weeks using fetal nuchal translucency, maternal serum free beta-human chorionic gonadotropin and pregnancy-associated plasma protein-A. Ultrasound Obstet Gynecol 1999 Apr;13(4):231-7.
17. Lawrence JB, Oxvig C, Overgaard MT, Sottrup-Jensen L, Gleich GJ, Hays LG, et al. The insulin-like growth factor (IGF)-dependent IGF binding protein-4 protease secreted by human fibroblasts is pregnancy-associated plasma protein-A. Proc Natl Acad Sci U S A 1999 Mar 16;96(6):3149-53.
18. Dugoff L, Hobbins JC, Malone FD, Porter TF, Luthy D, Comstock CH, et al. First-trimester maternal serum PAPP-A and free-beta subunit human chorionic gonadotropin concentrations and nuchal translucency are associated with obstetric complications: a population-based screening study (the FASTER Trial). Am J Obstet Gynecol 2004 Oct;191(4):1446-51.
19. Smith GC, Stenhouse EJ, Crossley JA, Aitken DA, Cameron AD, Connor JM. Early pregnancy levels of pregnancy-associated plasma protein a and the risk of intrauterine growth restriction, premature birth, preeclampsia, and stillbirth. J Clin Endocrinol Metab 2002 Apr;87(4):1762-7.
20. Levine RJ, Lam C, Qian C, Yu KF, Maynard SE, Sachs BP, et al. Soluble endoglin and other circulating antiangiogenic factors in preeclampsia. N Engl J Med 2006 Sep 7;355(10):992-1005.
21. Nucci M, Poon LC, Demirdjian G, Darbouret B, Nicolaides KH. Maternal serum placental growth factor (PlGF) isoforms 1 and 2 at 11-13 weeks' gestation in normal and pathological pregnancies. Fetal Diagn Ther 2014;36(2):106-16.
22. Yang W, Ahn H, Hinrichs M, Torry RJ, Torry DS. Evidence of a novel isoform of placenta growth factor (PlGF-4) expressed in human trophoblast and endothelial cells. J Reprod Immunol 2003 Oct;60(1):53-60.
23. Levine RJ, Maynard SE, Qian C, Lim KH, England LJ, Yu KF, et al. Circulating angiogenic factors and the risk of preeclampsia. N Engl J Med 2004 Feb 12;350(7):672-83.
24. Saffer C, Olson G, Boggess KA, Beyerlein R, Eubank C, Sibai BM. Determination of placental growth factor (PlGF) levels in healthy pregnant women without signs or symptoms of preeclampsia. Pregnancy Hypertens 2013 Apr;3(2):124-32.
25. Akolekar R, Zaragoza E, Poon LC, Pepes S, Nicolaides KH. Maternal serum placental growth factor at 11 + 0 to 13 + 6 weeks of gestation in the prediction of pre-eclampsia. Ultrasound Obstet Gynecol 2008 Nov;32(6):732-9.
26. Park F, Russo K, Williams P, Pelosi M, Puddephatt R, Walter M, et al. Prediction and prevention of early-onset pre-eclampsia: impact of aspirin after first-trimester screening. Ultrasound Obstet Gynecol 2015 Oct;46(4):419-23.
27. Rolnik DL, Wright D, Poon LC, O'Gorman N, Syngelaki A, de Paco MC, et al. Aspirin versus Placebo in Pregnancies at High Risk for Preterm Preeclampsia. N Engl J Med 2017 Jun 28.
28. Donalson K, Turner S, Morrison L, Liitti P, Nilsson C, Cuckle H. Maternal serum placental growth factor and alpha-fetoprotein testing in first trimester screening for Down syndrome. Prenat Diagn 2013 May;33(5):457-61.
29. Kagan KO, Hoopmann M, Abele H, Alkier R, Luthgens K. First-trimester combined screening for trisomy 21 with different combinations of placental growth factor, free beta-human chorionic gonadotropin and pregnancy-associated plasma protein-A. Ultrasound Obstet Gynecol 2012 Nov;40(5):530-5.
30. Zaragoza E, Akolekar R, Poon LC, Pepes S, Nicolaides KH. Maternal serum placental growth factor at 11-13 weeks in chromosomally abnormal pregnancies. Ultrasound Obstet Gynecol 2009 Apr;33(4):382-6.
31. Akolekar R, de CJ, Foidart JM, Munaut C, Nicolaides KH. Maternal plasma soluble fms-like tyrosine kinase-1 and free vascular endothelial growth factor at 11 to 13 weeks of gestation in preeclampsia. Prenat Diagn 2010 Mar;30(3):191-7.
32. Aggarwal PK, Chandel N, Jain V, Jha V. The relationship between circulating endothelin-1, soluble fms-like tyrosine kinase-1 and soluble endoglin in preeclampsia. J Hum Hypertens 2012 Apr;26(4):236-41.
33. Haggerty CL, Seifert ME, Tang G, Olsen J, Bass DC, Karumanchi SA, et al. Second trimester anti-angiogenic proteins and preeclampsia. Pregnancy Hypertens 2012 Apr 1;2(2):158-63.
34. Rana S, Powe CE, Salahuddin S, Verlohren S, Perschel FH, Levine RJ, et al. Angiogenic factors and the risk of adverse outcomes in women with suspected preeclampsia. Circulation 2012 Feb 21;125(7):911-9.
35. Zeisler H, Llurba E, Chantraine F, Vatish M, Staff AC, Sennstrom M, et al. Predictive Value of the sFlt-1:PlGF Ratio in Women with Suspected Preeclampsia. N Engl J Med 2016 Jan 7;374(1):13-22.
36. Scazzocchio E, Crovetto F, Triunfo S, Gratacos E, Figueras F. Validation of a first-trimester screening model for pre-eclampsia in an unselected population. Ultrasound Obstet Gynecol 2017 Feb;49(2):188-93.
The following are the partners of PRESIDE:
Copyright © Stefan Wagner - PRESIDE PROJECT